A guide to adverse drug reaction reporting
Adverse drug reaction reporting is an essential part of pharmacovigilance. It helps regulators to identify, assess, and address any potential safety risks of available medicines – and protect patient safety.
In this guide we explain who can report adverse drug reactions in the UK. We also take a deeper look at the adverse drug reaction reporting process, and outline how the process differs in the USA compared to the UK.
Please complete the form at the bottom of this article to request a complimentary trial of MedicinesComplete.
What is an adverse drug reaction?
An adverse drug reaction (ADR) is defined as a noxious, unintended response to a medicine. While some are relatively minor, others can be life-altering or even fatal.¹
ADRs are different from side effects, which tend to be more predictable. It is well established, for example, that diarrhoea and sickness are potential side effects of many antibiotics.²
Monitoring the occurrence of ADRs in available medicines is part of pharmacovigilance. It helps to protect patient safety.
All new drugs go through extensive testing before being licensed for use. Yet, clinical trials tend to involve a few thousand carefully selected patients at most. Some ADRs, however, may not become apparent until hundreds of thousands of people have used the medicine.³
Ongoing monitoring and reporting of all suspected ADRs—referred to as post-marketing surveillance—is vital for identifying rare adverse reactions and ensuring that appropriate action is taken.³
Who can report an ADR?
In the United Kingdom, the Medicines and Healthcare products Regulatory Agency (MHRA) encourages all health professionals (including students), patients, parents, and caregivers to report suspected ADRs to the Yellow Card scheme.
Reporting is voluntary. However, the Royal Pharmaceutical Society recommends pharmacists report all serious suspected ADRs they encounter as a matter of best practice – even if the effect is well recognised, and all suspected reactions to those products under additional monitoring (▼).⁵
It is important for health professionals to also encourage patients to self-report to the MHRA’s Yellow Card scheme as this helps them to understand better how an adverse effect has impacted their quality of life. The Yellow Card scheme database can detect duplicate reports, so do not hesitate to submit a report if you think the patient has already or vice versa. Hearing both perspectives is incredibly valuable when conducting safety investigations into incidents.

Which bodies are involved in ADR reporting?
The MHRA is the legislated regulator that monitors the safety of healthcare products, including suspected ADRs across the UK. MHRA collects and analyses Yellow Card reports, with the aim of detecting safety signals for investigation, and works with partners to assess the risk and take action where necessary.
#MedSafetyWeek
The Uppsala Monitoring Centre (UMC) collects and analyses ADR information worldwide and reports are sent to them by global regulators. It also leads the annual #MedSafetyWeek, a global social media campaign that encourages the reporting of suspected side effects and ADRs. In 2024, the MHRA was one of more than 90 organisations around the world to take part.⁶ This year’s event, to be held from 3 – 9 November, will mark the campaign’s 10th anniversary.⁷
When should I report a suspected ADR?
ADRs can arise from medicines that are used within or outside the terms of its licence. This includes licenced use, overdose, off-label use, misuse or abuse, and medication errors. Occupational exposure can also lead to an ADR.⁸
In general, health professionals should report all suspected adverse reactions where there is at least a reasonable possibility of causal relationship between the medicine and the reaction.⁹
All potential ADRs, no matter how minor, occurring with the use of a Black Triangle medicine should be reported.³
The Black Triangle Scheme from the MHRA collects data on selected medicines and vaccines after they reach the market. It was designed to intensively monitor the safety of innovative new treatments to ensure that their benefits continue to outweigh their risks.³ A black triangle (▼) is assigned to medicines or vaccines that contain a new active substance or combination, are administered via a new route or delivery system, or are well-established but used in a new patient population.³
How do I identify a potential ADR?
ADRs may become apparent during conversations with the patient. People may, for example, describe symptoms or concerns that indicate an adverse reaction. Abnormal clinical measures or laboratory results while on therapy may also be signs of an issue.⁹
Where do I report an ADR?
In the UK, ADR reports should be made to the MHRA’s Yellow Card scheme. The programme acts as an early warning system that signals if the safety of a product may require further investigation.¹⁰
Reports can be made for reactions to medicines in everyday use, including vaccines, blood factors and immunoglobins, complementary medicines, and safety issues with medical devices. Defective or low-quality medicine, falsified medicines or devices, and e-cigarette products also fall under the scheme’s remit.¹¹
How to make a report: Adverse drug reaction reporting form
The Yellow Card reporting form is issued by the MHRA. It covers all the information required to make an ADR report. Reporting is done electronically either via the Yellow Card website or via the Yellow Card app, which is free to download from iTunes or Google Play.
Reporting is also integrated into some clinical systems such as Optum (previously known as EMIS), SystmOne, Vision, MiDatabank, and Ulysses.¹²
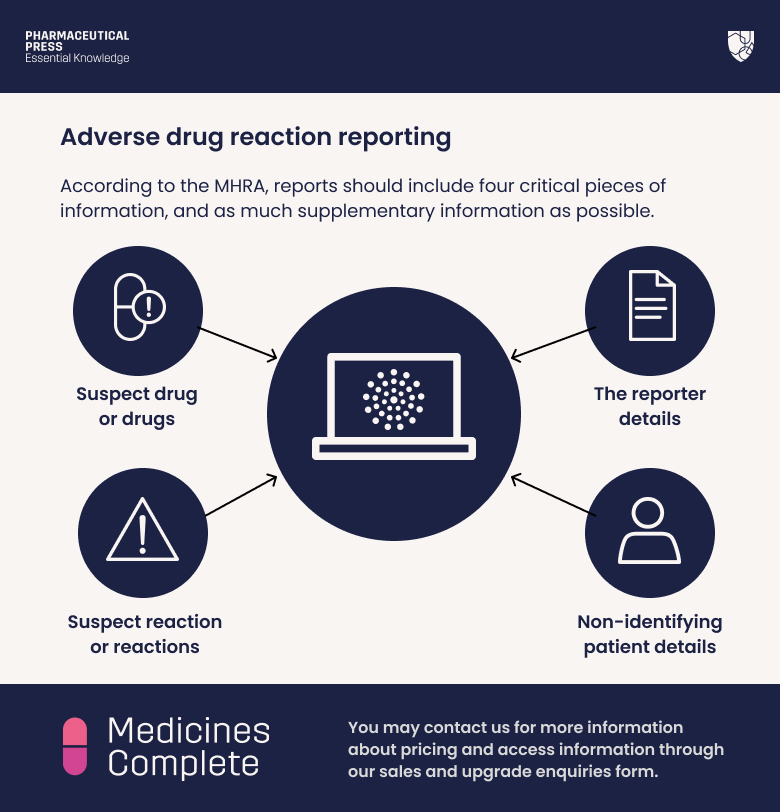
According to the MHRA, reports should include four critical pieces of information, and as much supplementary information as possible:¹³
1) Suspect drug or drugs
Supplementary information: Route of administration; dose, dose frequency, and schedule; date or dates of administration. When the report relates to a vaccine, reporters should, if possible, include the brand and batch number.
2) Suspect reaction or reactions
Supplementary information: When the reaction occurred; severity of the reaction; any treatment given for the reaction, and the outcome.
3) Non-identifying patient details
Reports should include the patient’s sex and/or age at the time of the reaction, along with, if known, their weight. The patient’s initials and a local identification code, such as a hospital or practice reference number, can help with identification in any future correspondence.
4) The reporter details
The reporter should include their name and contact details. This will allow the MHRA to acknowledge receipt and follow up if necessary.
Where possible, reporters should also include:¹³
• Any other drugs the patient has taken in the three months prior to the reaction, including over-the-counter and herbal medicines
• Where relevant, any information on further ADRs or issues with reintroduction of the drug
• Any relevant medical history, such as allergies
• Any relevant test results
• If the report is associated with congenital abnormalities, the MHRA asks reporters to list all other drugs taken during the pregnancy, as well as the date of the mother’s last menstrual period.
What happens to a Yellow Card report?
All reports are promptly entered into a database, which is subject to statistical analysis.⁹
Any potential safety signals are assessed by a group of scientists, physicians, and pharmacists. They evaluate the likelihood of a causal relationship between the drug and reaction. They also look to identify possible risk factors, such as age, underlying disease, or genetic susceptibility.⁹
The MHRA combines this information with that from other sources. This includes epidemiological studies, published and unpublished data, and pharmaceutical company safety updates, as well as data from other regulatory authorities and the Clinical Practice Research Datalink.⁹
Signals determined to warrant further action are discussed with experts, including MHRA epidemiologists and clinicians, and the Commission on Human Medicines and Expert Advisory Groups.⁹
If the evidence demonstrates a causal relationship between the medicine and the ADR, the MHRA takes action.⁹
This may take a variety of forms. It may involve, for example, adding the adverse effect to the drug’s label, changing the dosing recommendations, or issuing precaution advice. The MHRA may change the drug’s supply arrangements, for example, moving it from over-the-counter to prescription only, or subject it to additional monitoring requirements. In rare cases, where the risks are deemed to outweigh the benefits, the medicine may be removed from the market.⁹
ADR reporting in the USA
In the United States, the Food and Drug Administration (FDA) runs similar pharmacovigilance programmes to the MHRA’s Yellow Card Scheme.
ADR reports regarding medicines are made to MedWatch, while those relating to vaccines are sent to the Vaccine Adverse Event Reporting System (VAERS).¹⁴
Protecting patient safety
ADR monitoring is an essential part of pharmacovigilance, and health professionals have a critical role to play.
Timely and comprehensive reporting enables regulators to quickly identify emerging concerns and, importantly, take appropriate action.
Ultimately, it is about enhancing drug safety, safeguarding patient well-being, and improving healthcare outcomes.
Trial form
Please complete the form below to request a complimentary trial to knowledge products through MedicinesComplete.
References
1 European Medicines Agency. (n.d.). Adverse drug reaction. Available at: https://www.ema.europa.eu/en/glossary-terms/adverse-drug-reaction Last accessed: 30 September 2024
2 IU Phar. (n.d.). Adverse drug reactions. Available at: https://www.pharmacologyeducation.org/clinical-pharmacology/adverse-drug-reactions Last accessed: 6 March 2025
3 MHRA (2014). The Black Triangle Scheme (▼ or ▼*). Available at: https://www.gov.uk/drug-safety-update/the-black-triangle-scheme-or Last accessed: 6 March 2025
4 MHRA (2018). Suspect an adverse reaction? Yellow Card it! Available at: https://www.gov.uk/drug-safety-update/suspect-an-adverse-reaction-yellow-card-it Last accessed: 6 March 2025
5 Royal Pharmaceutical Society. (2024) Reporting adverse events. Medicines, Ethics and Practice 47 Available at: https://www.rpharms.com/mep/2-core-concepts-and-skills/25-patient-safety/253-reporting-adverse-events Last accessed: 6 March 2025
6 MHRA. (2024). #MedSafetyWeek. Available at: https://yellowcard.mhra.gov.uk/MedSafetyWeek Last accessed: 6 March 2025.
7 UMC. (2024) #MedSafetyWeek. Available at: https://who-umc.org/medsafetyweek/ Last accessed: 6 March 2025
8 MHRA. (n.d). Pharmacovigilance: The inside track. Available at: https://www.sps.nhs.uk/wp-content/uploads/2021/09/2021-10-13-circulation-MUS-Webinar-Pharmacovigilance-The-inside-track.pdf Last accessed: 6 March 2025
9 MHRA. (n.d.). Guidance on adverse drug reactions. Available at: https://assets.publishing.service.gov.uk/media/5feefb4c8fa8f53b7a0fbe36/Guidance_on_adverse_drug_reactions.pdf Last accessed: 6 March 2025
10 MHRA. (n.d.) What happens after you report? Available at: https://yellowcard.mhra.gov.uk/what-happens-report Last accessed: 6 March 2025
11 MHRA. (n.d.) About the Yellow Card scheme. Available at: https://yellowcard.mhra.gov.uk/about-yellow-card Last accessed: 6 March 2025
12 Joint Formulary Committee. British National Formulary (online) London: BMJ and Pharmaceutical Press. Available at: http://www.medicinescomplete.com Last accessed: 8 April 2025
13 MHRA. (n.d.). What to include in your Yellow Card of an adverse drug reaction. Available at: https://assets.publishing.service.gov.uk/media/5a81b671e5274a2e87dbf1c1/What_to_include_in_your_Yellow_Card_of_an_adverse_drug_reaction.pdf Last accessed: 6 March 2025
14 FDA. (n.d.) MedWatch forms for FDA safety reporting. Available at: https://www.fda.gov/safety/medical-product-safety-information/medwatch-forms-fda-safety-reporting Last accessed: 6 March 2025